LYCHEE ACUPUNCTURE CLINIC, INC.
Ph: 414-962-5577 - Dr. Lizhi Wei, L.Ac., Dipl.Ac. - 155 E Silver Spring Dr Whitefish Bay, WI 53217
Wednesday, May 27, 2015
Video: On the job with an animal acupuncturist
Video: On the job with an animal acupuncturist
Dr. Yanhui Qi says some people are skeptical when they first bring their animals in for acupuncture treatments at his Calgary clinic. Qi says he enjoys helping dogs, cats and horses using holistic veterinary techniques.
Sunday, May 24, 2015
Acupuncture Anti-Inflammatory Crohn’s Disease Discovery
Acupuncture Anti-Inflammatory Crohn’s Disease Discovery
HealthCMi on 23 May 2015.
Acupuncture reduces intestinal inflammation in patients with Crohn’s disease, reverses tissue damage, and improves the quality of life. Until now, how acupuncture achieves these results has gone unanswered. 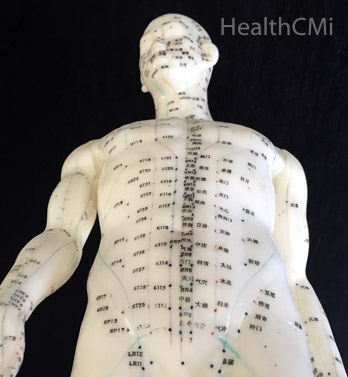 Researchers sought to solve this mystery and came up with concrete answers. With the help of immunohistochemistry, researchers discovered how acupuncture works for these patients.
Researchers sought to solve this mystery and came up with concrete answers. With the help of immunohistochemistry, researchers discovered how acupuncture works for these patients.
Crohn’s disease is an inflammatory bowel disease (IBD) characterized by abdominal pain, diarrhea, intestinal obstructions, abdominal masses, fatigue, nausea, mouth ulcers, and many other disruptions of the gastrointestinal system. Demographically, it disproportionately affects Scandinavians and Ashkenazim Jewish people. Crohn’s disease often affects the colon, anus, and terminal ileum (the distal aspect of the small intestine connecting to the cecum). Deep intestinal ulcerations with a patchy distribution throughout the gastrointestinal system help to distinguish Crohn’s disease from ulcerative colitis. Crohn’s disease has a serpiginous distribution of inflammation whereas ulcerative colitis has a contiguous distribution of inflammation.
Acupuncture and moxibustion have been shown to improve CDAI (Crohn’s Disease Activity Index) scores in modern research. CDAI scores are a method of measuring clinical responses to medicine and medical procedures by quantifying responses and remissions of Crohn’s disease. The researchers note that studies show that acupuncture improves CDAI scores, quality of life, increases hemoglobin levels, and reduces CRP levels for Crohn’s disease patients.
CRP (C-reactive protein) is determined by a blood test and quantifies inflammation levels. High levels indicate inflammation, often due to infections and chronic disease. The research demonstrates that acupuncture significantly lowers CRP levels for Crohn’s disease patients. With the help of an Olympus flourescent microscope, the researchers learned how acupuncture and moxibustion induce a powerful anti-inflammatory response in human patients with Crohn’s disease.
A confirmation of acupuncture and moxibustion’s benefits became apparent in a before and after intestinal biopsy comparison. Prior to acupuncture and moxibustion, patients had a significantly elevated level of giant, multinucleated cells in granulomas. Inflammatory and necrotic cells infiltrated the center of the granulomas. The mucosa epithelium was either damaged or completely absent. Lymphocytes infiltrated the lamina propria and intestinal glands were damaged. The glands contained necrotic, inflammatory, and multinucleated giant cells. After acupuncture and moxibustion, significant improvements were documented. The researchers note that the “intestinal mucosal epithelium was intact, the intestinal glands were reorganized, and less inflammatory cells infiltrated.”
The researchers carefully mapped the biological mechanisms regulated by acupuncture and moxibustion that achieved successful clinical results. What they discovered was that acupuncture and moxibustion induce a homeostatic response on the cellular level. Acupuncture and moxibustion relieved intestinal inflammation by regulating the ratio of inflammatory response cells. Proinflammatory Th17 cells and anti-inflammatory Treg cells were restored to normal levels and intestinal inflammation subsequently reduced. The researchers note this “study shows that moxibustion and acupuncture can reduce the number of Th17 cells and downregulate the expression of Th17-related molecules IL-17 and RORγt and increase the number of Treg cells and upregulate the expression of Treg transcription factor FOXP3 in the intestinal mucosa of CD (Chron’s disease) patients.” They add, “The present study showed that moxibustion and acupuncture can regulate and restore the balance between Th17 and Treg cells in intestinal mucosa of patients with CD."
The randomized study compared the results of acupuncture and moxibustion against a sham-placebo control group to ensure the validity of the results. Imaging, endoscopy, and histopathological exams confirmed the results. The research team shared the exact acupuncture and moxibustion procedures used to achieve clinical success. First, let’s look at the cellular changes induced by acupuncture and moxibustion. Next, we go over the exact acupuncture and moxibustion treatment protocol that helped the patients.
Citing Hovhannisyan et al., the researchers note, “An imbalance between Th17 and Treg cells constituted a key step in the disruption of intestinal homeostasis and is one of the major contributors to the development and progression of CD (Crohn’s disease).” TH17 (T helper 17) cells exert proinflammatory responses while Tregs (regulatory T cells, suppressor T cells) exert anti-inflammatory responses, especially in the case of auto-immune disorders. Crohn’s disease, which is often understood as an autoimmune disease, is characterized by unregulated proinflammatory responses. The study documents that acupuncture and moxibustion regulate the cells thereby balancing proinflammatory and anti-inflammatory responses.
The RORγt protein promotes differentiation of cells into proinflammatory Th17 cells. TH17 cells secrete proinflammatory cytokines including IL-17, which creates powerful proinflammatory responses. This causes neutrophils to migrate towards infections as part of the inflammatory cascade. Acupuncture and moxibustion downregulate IL17, RORγt, and TH17 cells.
The researchers add that “Th17 cells are the major contributor to inflammation in CD (Crohn’s disease)” and IL-17 is positively correlated with Crohn’s disease severity. This study demonstrates that acupuncture and moxibustion “reduced the number of TH17 cells and inhibited the expression of TH17-related molecules IL-17 and RORγt in the intestinal mucosa. It also increased the number of Treg cells and the expression of Treg-specific transcription factor FOXP3, thus restoring the ratio of the two cell types."
The researchers note that “a reduction in the number or function of Treg cells might be a major cause of the pathogenesis of Crohn’s disease. Tregs can suppress intestinal mucosal inflammation induced by innate or acquired immunity. FOXP3 and IL-2 promote the differentiation of Treg cells. Reduced numbers of Treg cells and deficiency in their function can cause damage in the intestinal mucosa, resulting in CD (Crohn’s disease).” Tregs can inhibit the proliferation of Th cells and subsequent production of inflammatory factors although they may differentiate into Th17 cells in other instances. Research demonstrates that reduced Tregs and FOXP3 in the bloodstream are correlated with Crohn’s disease. Moreover, the ratio of Treg to Th17 cells both in the intestinal mucosa and peripheral bloodstream is reduced in patients with Crohn’s disease. The researchers note that “restoring the balance between these cells is essential for the treatment of intestinal inflammation in CD.” Acupuncture and moxibustion restored the balance between these cells and testing also revealed significant positive patient clinical improvements.
Treatment
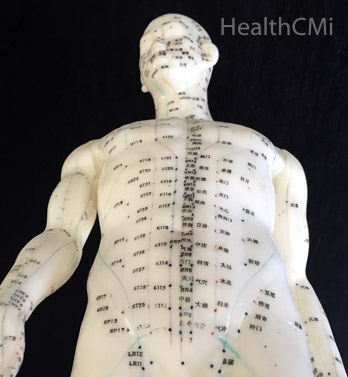
Acupuncture was administered at the following acupoints:
Moxibustion was administered at the following acupoints:
http://www.healthcmi.com/Acupuncture-Continuing-Education-News/1478-acupuncture-anti-inflammatory-crohn-s-disease-discovery
 Researchers sought to solve this mystery and came up with concrete answers. With the help of immunohistochemistry, researchers discovered how acupuncture works for these patients.
Researchers sought to solve this mystery and came up with concrete answers. With the help of immunohistochemistry, researchers discovered how acupuncture works for these patients.Crohn’s disease is an inflammatory bowel disease (IBD) characterized by abdominal pain, diarrhea, intestinal obstructions, abdominal masses, fatigue, nausea, mouth ulcers, and many other disruptions of the gastrointestinal system. Demographically, it disproportionately affects Scandinavians and Ashkenazim Jewish people. Crohn’s disease often affects the colon, anus, and terminal ileum (the distal aspect of the small intestine connecting to the cecum). Deep intestinal ulcerations with a patchy distribution throughout the gastrointestinal system help to distinguish Crohn’s disease from ulcerative colitis. Crohn’s disease has a serpiginous distribution of inflammation whereas ulcerative colitis has a contiguous distribution of inflammation.
Acupuncture and moxibustion have been shown to improve CDAI (Crohn’s Disease Activity Index) scores in modern research. CDAI scores are a method of measuring clinical responses to medicine and medical procedures by quantifying responses and remissions of Crohn’s disease. The researchers note that studies show that acupuncture improves CDAI scores, quality of life, increases hemoglobin levels, and reduces CRP levels for Crohn’s disease patients.
CRP (C-reactive protein) is determined by a blood test and quantifies inflammation levels. High levels indicate inflammation, often due to infections and chronic disease. The research demonstrates that acupuncture significantly lowers CRP levels for Crohn’s disease patients. With the help of an Olympus flourescent microscope, the researchers learned how acupuncture and moxibustion induce a powerful anti-inflammatory response in human patients with Crohn’s disease.
A confirmation of acupuncture and moxibustion’s benefits became apparent in a before and after intestinal biopsy comparison. Prior to acupuncture and moxibustion, patients had a significantly elevated level of giant, multinucleated cells in granulomas. Inflammatory and necrotic cells infiltrated the center of the granulomas. The mucosa epithelium was either damaged or completely absent. Lymphocytes infiltrated the lamina propria and intestinal glands were damaged. The glands contained necrotic, inflammatory, and multinucleated giant cells. After acupuncture and moxibustion, significant improvements were documented. The researchers note that the “intestinal mucosal epithelium was intact, the intestinal glands were reorganized, and less inflammatory cells infiltrated.”
The researchers carefully mapped the biological mechanisms regulated by acupuncture and moxibustion that achieved successful clinical results. What they discovered was that acupuncture and moxibustion induce a homeostatic response on the cellular level. Acupuncture and moxibustion relieved intestinal inflammation by regulating the ratio of inflammatory response cells. Proinflammatory Th17 cells and anti-inflammatory Treg cells were restored to normal levels and intestinal inflammation subsequently reduced. The researchers note this “study shows that moxibustion and acupuncture can reduce the number of Th17 cells and downregulate the expression of Th17-related molecules IL-17 and RORγt and increase the number of Treg cells and upregulate the expression of Treg transcription factor FOXP3 in the intestinal mucosa of CD (Chron’s disease) patients.” They add, “The present study showed that moxibustion and acupuncture can regulate and restore the balance between Th17 and Treg cells in intestinal mucosa of patients with CD."
The randomized study compared the results of acupuncture and moxibustion against a sham-placebo control group to ensure the validity of the results. Imaging, endoscopy, and histopathological exams confirmed the results. The research team shared the exact acupuncture and moxibustion procedures used to achieve clinical success. First, let’s look at the cellular changes induced by acupuncture and moxibustion. Next, we go over the exact acupuncture and moxibustion treatment protocol that helped the patients.
Citing Hovhannisyan et al., the researchers note, “An imbalance between Th17 and Treg cells constituted a key step in the disruption of intestinal homeostasis and is one of the major contributors to the development and progression of CD (Crohn’s disease).” TH17 (T helper 17) cells exert proinflammatory responses while Tregs (regulatory T cells, suppressor T cells) exert anti-inflammatory responses, especially in the case of auto-immune disorders. Crohn’s disease, which is often understood as an autoimmune disease, is characterized by unregulated proinflammatory responses. The study documents that acupuncture and moxibustion regulate the cells thereby balancing proinflammatory and anti-inflammatory responses.

The RORγt protein promotes differentiation of cells into proinflammatory Th17 cells. TH17 cells secrete proinflammatory cytokines including IL-17, which creates powerful proinflammatory responses. This causes neutrophils to migrate towards infections as part of the inflammatory cascade. Acupuncture and moxibustion downregulate IL17, RORγt, and TH17 cells.
The researchers add that “Th17 cells are the major contributor to inflammation in CD (Crohn’s disease)” and IL-17 is positively correlated with Crohn’s disease severity. This study demonstrates that acupuncture and moxibustion “reduced the number of TH17 cells and inhibited the expression of TH17-related molecules IL-17 and RORγt in the intestinal mucosa. It also increased the number of Treg cells and the expression of Treg-specific transcription factor FOXP3, thus restoring the ratio of the two cell types."
The researchers note that “a reduction in the number or function of Treg cells might be a major cause of the pathogenesis of Crohn’s disease. Tregs can suppress intestinal mucosal inflammation induced by innate or acquired immunity. FOXP3 and IL-2 promote the differentiation of Treg cells. Reduced numbers of Treg cells and deficiency in their function can cause damage in the intestinal mucosa, resulting in CD (Crohn’s disease).” Tregs can inhibit the proliferation of Th cells and subsequent production of inflammatory factors although they may differentiate into Th17 cells in other instances. Research demonstrates that reduced Tregs and FOXP3 in the bloodstream are correlated with Crohn’s disease. Moreover, the ratio of Treg to Th17 cells both in the intestinal mucosa and peripheral bloodstream is reduced in patients with Crohn’s disease. The researchers note that “restoring the balance between these cells is essential for the treatment of intestinal inflammation in CD.” Acupuncture and moxibustion restored the balance between these cells and testing also revealed significant positive patient clinical improvements.
Treatment
Acupuncture was administered at the following acupoints:
- Zusanli (ST36)
- Shangjuxu (ST37)
- Sanyinjiao (SP6)
- Taixi (KI3)
- Gongsun (SP4)
- Taichong (LR3)
Moxibustion was administered at the following acupoints:
- Tianshu (ST25)
- Qihai (CV6)
- Zhongwan (CV12)
- Coptis chinensis (Huang Lian)
- Radix Aconiti Lateralis (Fu Zi, aconite)
- Cortex Cinnamomi (Rou Gui, cinnamon bark)
- Radix Aucklandiae (Mu Xiang)
- Flos carthami (Hong Hua, saffron)
- Salvia miltiorrhiza (Dan Shen)
- Angelica sinensis (Dang Gui)
http://www.healthcmi.com/Acupuncture-Continuing-Education-News/1478-acupuncture-anti-inflammatory-crohn-s-disease-discovery
Labels:
acupoints,
Acupucture,
Acupucture article,
Crohn’s Disease,
Moxibustion
Saturday, May 23, 2015
A wellness approach to treating anxiety - Bangor Daily News (Maine, USA)
Dr. Michael Noonan
Anxiety is becoming increasingly common, as are the drugs prescribed for it. Like any complex health problem, anxiety is best seen as a condition that has many causes.It appears that while there are hereditary tendencies toward anxiety, for most of us it does not become a problem unless triggered, typically by our lifestyles. While it is quite common — 18 percent of the adult population is affected by it every year — only about 4 percent of the population is severely impacted by the disease.
Anxiety sometimes is described as an imbalance in the chemistry of the brain. The biggest influence on our brain chemistry is our diet. A healthy brain balance is supported by — this should be a surprise to no one — a healthy diet. Highly processed foods, artificial flavorings and preservatives, crops raised on chemicals instead of fertile soil and animals raised on grains instead of their natural foods all affect our brains. This especially is true of sugar, which causes a blood sugar “spike” and then a “crash” that stresses our systems, including the brain.
The dietary recommendations for anxiety are the same for diabetes, heart disease, obesity, etc. Eat whole, minimally processed, preferably organic foods and avoid or at least limit “non-foods,” such as soda, chips, ice cream and pastries.
Of course, chronic stress is a huge trigger for anxiety. Over time, the effects of stress build up in the body; if it is not released somehow, it can become a problem. Exercise is one of the best ways to address this problem; just walking 30 minutes per day helps. Doing just the opposite — sitting quietly, without the computer or TV on, for 5 minutes, then gradually working your way up to 10 minutes or more — can go a long way toward easing this build up of stress and anxiety.
On the treatment side, plenty of wellness options are available. In my experience, acupuncture is one of the most effective. There are many different approaches in acupuncture, ranging from using several needles throughout the body to using only a few select points or even treating only ear points. Auriculotherapy, acupuncture to the ears, has been increasingly used by the military with good results.
Not every patient reacts the same. Sometimes, a few styles have to be tried before the patient gets the full benefit.
There also are herbs used to control anxiety. One of the key benefits of herbals is the fact that they do not have serious side effects, like anti-anxiety medications. Their downside is poor quality control. In a recent report, the attorney general of New York had “off the shelf” herbal supplements tested from stores including Walmart, Target and GNC. A shocking 80 percent of the supplements had none of the active ingredients listed on the bottle. Contaminants also were found in the supplements. This is why I do not recommend buying herbals at a local store. I use a company that has their products extensively tested for quality and to ensure the dosage is consistent, and they provide information and training on proper usage, including drug interactions.
There is natural, drug-free help for many, if not most, anxiety sufferers. In my experience, the most severe cases seem to respond best to medication, but the majority of patients can control their symptoms naturally, with lifestyle changes and some wellness-based care.
http://bangordailynews.com/2015/05/21/health/blogs-and-columns/a-wellness-approach-to-treating-anxiety/
Sunday, May 17, 2015
Acupuncture Speeds Low Back Recovery
Acupuncture Speeds Low Back Recovery
HealthCMi on 15 May 2015.
Acupuncture speeds recovery from lumbar disc herniations. Researchers tested a protocol that increased the efficacy of electroacupuncture procedures for disc herniations by adding Chinese herbal medicine iontophoresis.  They discovered that the combined therapy of electroacupuncture plus herbal iontophoresis enhances clinical efficacy with a significant synergistic effect.
They discovered that the combined therapy of electroacupuncture plus herbal iontophoresis enhances clinical efficacy with a significant synergistic effect.
Patients had greater pain relief and lumbar functional improvements with the combination therapy. The total effective rate of electroacupuncture only was 87.5%. The combined therapy approach had a total effective rate of 95.0%. McGill and Japanese Orthopedic Association assessments using a Visual Analogue Scale (VAS) were used to calculate improvements.
A lumbar intervertebral disc herniation is a rupture of the annulus fibrosus that causes extrusion of the nucleus pulposus from the center of the disc. This often causes low back pain, weakness, or numbness that may radiate to the legs and feet. The researchers confirmed disc herniations for participants with diagnostic tests including CT scans, MRIs, and a positive Lasegue’s or Bragard’s sign. Patients were also evaluated with X-rays and an assessment of range of motion restrictions and pain levels. A total of 80 patients from the rehabilitation center at the Second Hospital Affiliated to Heilongjiang University of Traditional Chinese Medicine (TCM) participated in the study.
Acupuncture Points
The researchers used the following acupuncture points:
Disposable, single-use, sterile filiform needles of 0.30 mm diameter and a 40-75 mm length were used. Jiaji points were needled with 50 mm needles to a depth of approximately 40 mm. Needles were angled slightly towards the spine. Manual acupuncture was subsequently applied with an even reinforcing-reducing technique. The researchers note that the optimal response is if the patient reported a sensation radiating downwardly towards the buttocks and leg on the affected side. Electroacupuncture was then applied to the Jiaji points of the affected vertebral level. A sparse-dense setting was used with a 2 - 100 Hz frequency. Intensity was set to patient comfortability levels.
GB30 was needled using 75 mm needles and the remaining points were needled with 40 mm needles perpendicularly with the addition of the even reinforcing-reducing technique. The treatment duration was thirty minutes per acupuncture session. Acupuncture treatments were applied once per day for 10 days followed by a three day break from treatments. Next, another course of ten acupuncture treatments over ten days was applied for a total of two courses of care.
Acupuncture treatments were applied once per day for 10 days followed by a three day break from treatments. Next, another course of ten acupuncture treatments over ten days was applied for a total of two courses of care.
Chinese Herbs
Iontophoresis is the administration of a substance through the skin by using a direct electric current. An LD-AE thermal treatment device was used to apply the current to the Chinese medicinal herbs. The herbs used in the iontophoresis procedure were:
Findings
The researchers reviewed current studies and commented on a few aspects of acupuncture therapy. Citing Zhao et al., they note that Jiaji electroacupuncture improves microcirculation to affected regions, speeds cell metabolism, transforms or reduces inflammatory substances, and reduces edema. Citing Yan et al., the researchers note that electroacupuncture “can alleviate pain by inhibiting the pathological reaction in the cerebral cortex through increasing opioid peptide release of periphery inflammatory tissues.”
Citing several studies (Yang et al., Yuan et al., Li et al.), the researchers note that electroacupuncture “at contralateral Jiaji (EX-B2) points can help to eliminate aseptic inflammation in intervertebral space through the current impulse, alleviate inflammatory irritation, and relieve compression to the nerve root.” Citing Chen et al., they add that electroacupuncture accelerates tissue metabolism, nurtures tissues, and reduces edema by stimulating rhythmic muscle contractions. Citing Cai et al., the researchers note that iontophoresis of Chinese herbal medicine increases blood circulation, relaxes muscles, and increases the efficacy of electrotherapy.
Evaluation
The researchers note that “EA (electroacupuncture) at lumbar Jiaji (EX-B2) points combined with iontophoresis of Chinese medicine can obtain better analgesic effect than EA alone. In addition, the effect tends to increase with time.” They add that the combined therapeutic approach speeds recovery, improves lumbar functions, and improves the pain relief therapeutic efficacy.
http://www.healthcmi.com/Acupuncture-Continuing-Education-News/1467-acupuncture-speeds-low-back-recovery
 They discovered that the combined therapy of electroacupuncture plus herbal iontophoresis enhances clinical efficacy with a significant synergistic effect.
They discovered that the combined therapy of electroacupuncture plus herbal iontophoresis enhances clinical efficacy with a significant synergistic effect.Patients had greater pain relief and lumbar functional improvements with the combination therapy. The total effective rate of electroacupuncture only was 87.5%. The combined therapy approach had a total effective rate of 95.0%. McGill and Japanese Orthopedic Association assessments using a Visual Analogue Scale (VAS) were used to calculate improvements.
A lumbar intervertebral disc herniation is a rupture of the annulus fibrosus that causes extrusion of the nucleus pulposus from the center of the disc. This often causes low back pain, weakness, or numbness that may radiate to the legs and feet. The researchers confirmed disc herniations for participants with diagnostic tests including CT scans, MRIs, and a positive Lasegue’s or Bragard’s sign. Patients were also evaluated with X-rays and an assessment of range of motion restrictions and pain levels. A total of 80 patients from the rehabilitation center at the Second Hospital Affiliated to Heilongjiang University of Traditional Chinese Medicine (TCM) participated in the study.
Acupuncture Points
The researchers used the following acupuncture points:
- Jiaji (Ex-B2, affected vertebral levels, bilateral)
- GB30 (Huantiao, affected side)
- Ashi
- GB34 (Yanglingquan, affected side for L4-5 herniations)
- BL40 (Weizhong, affected side for L5-S1 herniations)
Disposable, single-use, sterile filiform needles of 0.30 mm diameter and a 40-75 mm length were used. Jiaji points were needled with 50 mm needles to a depth of approximately 40 mm. Needles were angled slightly towards the spine. Manual acupuncture was subsequently applied with an even reinforcing-reducing technique. The researchers note that the optimal response is if the patient reported a sensation radiating downwardly towards the buttocks and leg on the affected side. Electroacupuncture was then applied to the Jiaji points of the affected vertebral level. A sparse-dense setting was used with a 2 - 100 Hz frequency. Intensity was set to patient comfortability levels.
GB30 was needled using 75 mm needles and the remaining points were needled with 40 mm needles perpendicularly with the addition of the even reinforcing-reducing technique. The treatment duration was thirty minutes per acupuncture session.
 Acupuncture treatments were applied once per day for 10 days followed by a three day break from treatments. Next, another course of ten acupuncture treatments over ten days was applied for a total of two courses of care.
Acupuncture treatments were applied once per day for 10 days followed by a three day break from treatments. Next, another course of ten acupuncture treatments over ten days was applied for a total of two courses of care.Chinese Herbs
Iontophoresis is the administration of a substance through the skin by using a direct electric current. An LD-AE thermal treatment device was used to apply the current to the Chinese medicinal herbs. The herbs used in the iontophoresis procedure were:
- Qiang Huo (Rhizoma et Radix Notopterygii)
- Du Huo (Radix Angelicae Pubescentis)
- Xuan Shen (Radix Scrophulariae)
- Bi Xie (Rhizoma Dioscoreae Hypoglaucae)
- Sheng Di Huang (Radix Rehmanniae)
- Shu Di Huang (Radix Rehmanniae preparata)
- Dang Gui (Radix Angelicae Sinensis)
- Du Zhong (Cortex Eucommiae)
- Fang Feng (Radix Saposhnikoviae)
- Rou Gui (Cortex Cinnamomi)
- Gui Zhi (Ramulus Cinnamomi)
- Bai Zhi (Radix Angelicae Dahuricae)
- Ru Xiang (Olibanum)
- Mo Yao (Myrrha)
- Tian Ma (Rhizoma Gastrodiae)
Findings
The researchers reviewed current studies and commented on a few aspects of acupuncture therapy. Citing Zhao et al., they note that Jiaji electroacupuncture improves microcirculation to affected regions, speeds cell metabolism, transforms or reduces inflammatory substances, and reduces edema. Citing Yan et al., the researchers note that electroacupuncture “can alleviate pain by inhibiting the pathological reaction in the cerebral cortex through increasing opioid peptide release of periphery inflammatory tissues.”
Citing several studies (Yang et al., Yuan et al., Li et al.), the researchers note that electroacupuncture “at contralateral Jiaji (EX-B2) points can help to eliminate aseptic inflammation in intervertebral space through the current impulse, alleviate inflammatory irritation, and relieve compression to the nerve root.” Citing Chen et al., they add that electroacupuncture accelerates tissue metabolism, nurtures tissues, and reduces edema by stimulating rhythmic muscle contractions. Citing Cai et al., the researchers note that iontophoresis of Chinese herbal medicine increases blood circulation, relaxes muscles, and increases the efficacy of electrotherapy.
Evaluation
The researchers note that “EA (electroacupuncture) at lumbar Jiaji (EX-B2) points combined with iontophoresis of Chinese medicine can obtain better analgesic effect than EA alone. In addition, the effect tends to increase with time.” They add that the combined therapeutic approach speeds recovery, improves lumbar functions, and improves the pain relief therapeutic efficacy.
http://www.healthcmi.com/Acupuncture-Continuing-Education-News/1467-acupuncture-speeds-low-back-recovery
Wednesday, May 13, 2015
New Study on Acupuncture to Reduce Pain and Inflammation in Children with Acute Appendicitis
New Study on Acupuncture to Reduce Pain and Inflammation in Children with Acute Appendicitis
13 May 2015 Mary Ann Liebert, Inc., Publishers
Acupuncture was shown to lessen pain and reduce the underlying inflammation in pediatric patients with a diagnosis of acute appendicitis, according to a study published in The Journal of Alternative and Complementary Medicine, a peer-reviewed publication from Mary Ann Liebert, Inc., publishers (http://www.liebertpub.com). The article is available free on The Journal of Alternative and Complementary Medicine website until June 12, 2015.
Alan L. Nager, MD, MHA and coauthors from Children's Hospital Los Angeles and the Keck School of Medicine of the University of Southern California assessed subjective pain among pediatric patients immediately before and 20 minutes after treatment by a licensed acupuncturist. The researchers also measured two biomarkers of inflammation in blood samples taken before, during, and 30 minutes after needle placement.
In the article "Effects of Acupuncture on Pain and Inflammation in Pediatric Emergency Department Patients with Acute Appendicitis: A Pilot Study," the authors report that the patients' subjective pain decreased, likely due to the acupuncture treatment.. Furthermore, one of the inflammatory biomarkers (white blood cell count) "showed a modest and noticeable drop," suggesting "that the effectiveness of acupuncture may have a biophysiological basis."
http://online.liebertpub.com/doi/full/10.1089/acm.2015.0024
Labels:
Acupucture article,
Acute Appendicitis,
Children,
Inflammation,
Pain
Saturday, May 9, 2015
Comparison of the efficacy of diclofenac, acupuncture, and acetaminophen in the treatment of renal colic
Comparison of the efficacy of diclofenac, acupuncture, and acetaminophen in the treatment of renal colic - Abstract
Published: 08 May 2015
OBJECTIVE: The objective is to compare the analgesic effects of diclofenac, acetaminophen, and acupuncture in urolithiasis-driven renal colic pain relief.
RESULTS: No significant differences in baseline VAS or VRS were found with regard to age or sex. After 10 minutes, all 3 groups experienced a significant decrease in VAS and VRS scores, with the most drastic decrease occurring in group II. After 30 minutes, there was a significantly higher decrease in group III than in group I (P = .001). After 60 minutes, mean VAS scores of groups I and III (P = .753) were similar. The mean VAS score of group III was lower than that of group II (P = .013). After 120 minutes, the difference in the VAS scores was (P = .000) between groups I and II and between groups II and III. Yet, the VAS evaluation made after 120 minutes revealed statistically similar outcomes for groups I and III (P = .488). The statistical findings for VRS evaluations made after 10, 30, 60, and 120 were similar to those for VAS.
CONCLUSIONS: In renal colic patients with a possible nonsteroidal anti-inflammatory drug and acetaminophen side effect risk, acupuncture emerges as an alternative treatment modality.
Written by:
Kaynar M, Koyuncu F, Buldu İ, Tekinarslan E, Tepeler A, Karatağ T, İstanbulluoğlu MO, Ceylan K.
Department of Urology, Selcuk University, Faculty of Medicine, Konya, Turkey; Department of Emergency Medicine, Beyhekim State Hospital, Konya, Turkey; Department of Urology, Mevlana University, Faculty of Medicine, Konya, Turkey; Department of Urology, Konya Education and Research Hospital, Konya, Turkey; Department of Urology, Bezmialem Vakıf University, Faculty of Medicine, Istanbul,Turkey. mekaynar@gmail.com
Reference: Am J Emerg Med. 2015 Feb 25. pii: S0735-6757(15)00122-9.
doi: 10.1016/j.ajem.2015.02.033
PubMed Abstract
PMID: 25827597
UroToday.com Stone Disease Section
Wednesday, May 6, 2015
Acupuncture Effective for Post-Tonsillectomy Pain in Children
Acupuncture Effective for Post-Tonsillectomy Pain in Children
Last Updated: May 06, 2015. Less pain, analgesic drug consumption for children treated with acupuncture, standard analgesics | ||
Acupuncture, in addition to conventional analgesic treatment, is an effective treatment for post-tonsillectomy pain in children, according to a study published in the June issue of Pediatric Anesthesia.
WEDNESDAY, May 6, 2015 (HealthDay News) -- Acupuncture, in addition to conventional analgesic treatment, is an effective treatment for post-tonsillectomy pain in children, according to a study published in the June issue of Pediatric Anesthesia.
Peter Gilbey, M.D., from the Ziv Medical Center in Safed, Israel, and colleagues examined whether acupuncture, in addition to conventional analgesic treatment, would be effective for post-tonsillectomy pain in children. Sixty children, aged 3 to 12 years, undergoing tonsillectomy were randomized to receive conventional postoperative analgesic treatment or the same regimen plus acupuncture.
The researchers found that the children assigned to the acupuncture group had less pain and less analgesic drug consumption. In addition, the acupuncture group reported higher patient/parent satisfaction with analgesic treatment scores. There were no adverse effects recorded.
"Acupuncture is a safe treatment, well tolerated by children aged 3 to 12 years and by their parents," the authors write. "Additional studies are warranted to further evaluate the efficacy of acupuncture for postoperative and perhaps other pain relief. There is a need for further research regarding intraoperative acupuncture and the long-term analgesic effect of acupuncture."
http://www.doctorslounge.com/index.php/news/pb/55022
Subscribe to:
Posts (Atom)
